Coagulation (clotting) screen
| Category | Haematology |
|---|---|
| Test background |
The coagulation screen comprises PT, APTT and fibrinogen. Prothrombin time: (PT) used as a measure of the extrinsic pathway of coagulation and determines the clotting tendency of blood. PT measures factors I, II, V, VII and X • an abnormal PT suggests either a congenital or an acquired deficiency of a clotting factor in the extrinsic or common pathway • deficiencies can be acquired in liver disease, vitamin K deficiency or treatment with vitamin K antagonist drugs, ie. warfarin, sinthrome, dindevan or phenindione • if there is no suggestion of any of these deficiency states, a congenital deficiency should be considered • International Normalised Ratio (INR) is derived from the PT; it is used to monitor warfarin dosage and will only be reported where a patient is taking warfarin or other dicoumarol drug (see INR) Activated partial thromboplastin time (APTT): • a global screening procedure used primarily to evaluate coagulation abnormalities in the intrinsic pathway but will also detect severe functional deficiencies in factors II, V, X or fibrinogen • also widely advocated as a means to monitor the effectiveness of unfractionated heparin therapy, where the clotting time is prolonged in proportion to the level of heparin; this is normally reported as a ratio to the midpoint of the APTT reference range (see APTTR) • APTT and APTTR are inappropriate for monitoring low molecular weight heparin (LMWH) dosage; the anti Xa assay is normally used for monitoring LMWH (see HEPAXA) • in patients receiving oral anticoagulants, the circulating levels of factors II, VII, IX and X are reduced, therefore the APTT can be expected to be prolonged • the presence of non-specific inhibitors, such as lupus-like anticoagulant, may prolong the APTT, but this effect is variable and specific lupus anticoagulant testing should be requested where suspected (see lupus) • deficiencies of factors VIII, IX, XI and XII, and rarely von Willebrand factor (if causing a low factor VIII level), may lead to a prolonged APTT which will correct following mixing studies with normal plasma Fibrinogen: deficiencies of fibrinogen can indicate disseminated intravascular coagulation (DIC) or can be an indicator of bleeding problems or liver and renal dysfunction • reduced fibrinogen can also be seen after massive transfusion and is used as an indicator for the requirement of fresh frozen plasma • abnormal clotting findings may be followed by specific factor assays to enable differential diagnosis of acquired vs. inherited causes A thrombin time (TT): may be reported in a small number of cases where other coagulation screen parameters are abnormal, if deemed appropriate. |
| Clinical Indications |
Pre-operative screening where the patient’s personal or family history is suggestive of a coagulopathy Internal haemorrhage not related to trauma Prolonged bleeding of any cause Recurrent haemorrhage, eg. bleeding gums or epistaxis Recurrent spontaneous bruising Haemorrhage into unusual places, eg. joints (with no explanation) Acutely unwell patients in whom DIC is suspected, eg. septicaemia |
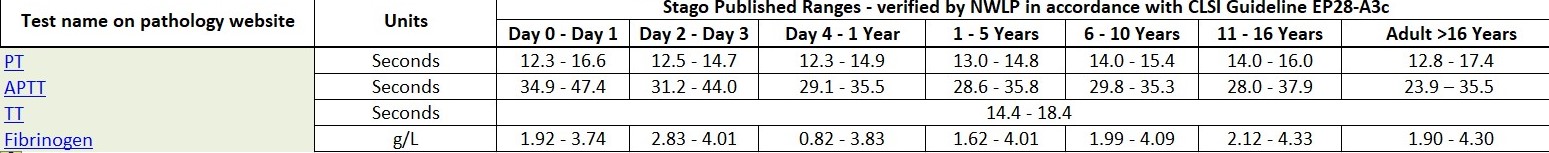
| Reference range |
|
| Sample & container required | 2.7 mL sodium citrate (pale blue top) adults 1.8 mL sodium citrate (pale blue top) paediatrics |
| Turnaround time | 4 hours |
| Notes | Special handling: avoid prolonged stasis during venepuncture. Sample must be received by lab within 4 hours of collection. Please note: samples will be rejected if underfilled or overfilled. Adult Reference Range: Note: The reference ranges for use on patients over the age of 16 years, has been locally verified in accordance with CLSI Guideline EP28-A3c through evaluation on representative normal individuals across the sites to reflect our patient population. Data sourced via Stago from: Paediatric Reference Range Note: Due to the complexity of collecting blood samples for analysis on normal neonates and paediatric patients, the reference ranges for use on patients up to 16 years of age have been taken from published data, from a research study using comparable methodology and equipment as that currently employed in our organisation. Please contact the laboratory for coagulation paediatric ranges. Data sourced via Stago from: |